Induction of labor is definitely a process. How long will your labor induction take? What should you expect? Pregnant women often wonder how long will it take until they give birth?
Before we get going, getting the RIGHT questions answered is SO important — grab my induction question checklist right here:
How long does it take to give birth after being induced?
Average time for an induction using cervical ripening agents is about 19 hours plus or minus 12 hours — as tallied in this study.
It depends on:
- Cervical readiness & Baby’s Position
- Prior vaginal deliveries
- How your body responds to the induction method(s)
So, it really depends — but I’m going to give you some ideas based on why/how you are being induced… so let me give you some more information (feel free to click to the area you’re interested in):
In this Article:
Things That Affect How Long Your Induction Will Take:
If you’re really interested I totally recommend checking out this study — you’ll see how specific variables effect how long the induction is.
Note: That study is done with those who had a Dinoprostone induction which means they were less than 3 cm when they started and used cervical ripening agents to get labor going.
Cervical Readiness: Your Bishop Score
Your cervical readiness is one of the most important parts of how well your body takes to an induction usually, although not always).
We qualify your cervical readiness as something called the “bishop score”. It measures how prepared your cervix is to open. It’s on a scale of 0 to 13. You don’t need to know your bishop score, but some hospitals won’t do an elective induction if your cervix isn’t open/soft enough.
What/Where is your Cervix?
Your Cervix is at the end of your vagina, it’s at the opening of your uterus.
Cervical Dilation
This means how OPEN your cervix is. I have a whole post that explains vaginal dilation on my sister site, but what you need to know is that as the baby progresses into your pelvis, the cervix opens. Kind of like when you push your head through a tight sweater neck.
The numbers go from 0 (or closed) to 10 (ten is actually when your cervix disappears behind the baby’s head).
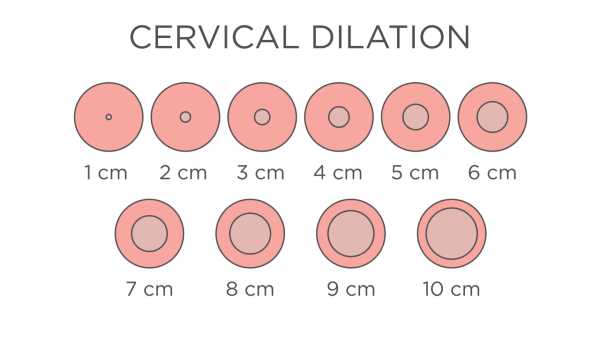
The more open your cervix is, it normally means your induction will be shorter. Which make sense, as you don’t start to push the baby out til’ 10 centimeters (cm).
Cervical Thinning
If you keep the “head through a sweater” analogy, you’ll know that the sweater thins at the neck as you pull your head through. The same thing happens with your cervix.
Medical providers measure this as a percentage. Anything more than 50% normally just called “thick” (frankly, it’s impossible for us to know how thick your cervix is in the beginning).
We CAN measure the length of your cervix but that is done by ulrasound, rather than our hand.
That all being said, if your cervix is thick, it normally takes longer until the baby comes out.
Baby’s Station
This measures how above or below your ischial spines (your butt bones) the baby is.
I think it’s easier to envision how high or low in your pelvis the baby is.
If the baby is high it will take longer for it to descend.
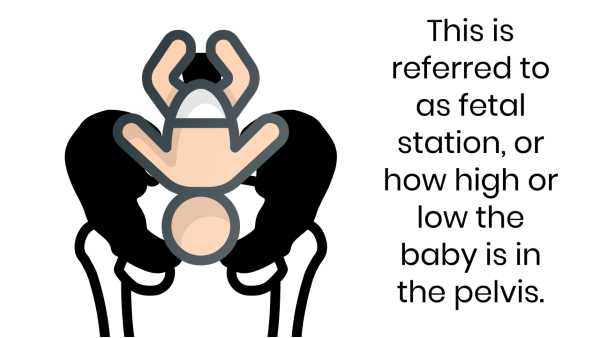
NORMALLY, the lower your baby is, the more it will start to open your cervix (again, as you push your head further into the sweater it opens more).
Consistancy of your Cervix
This means how firm or soft it is.
Early in pregnancy your cervix is hard and firm like rubber, then it softens up as you progress. If your cervix is hard we know that it will take a bit of labor in order for it to soften.
If it’s your first baby, you will normally have a firmer cervix than subsequent babies.
Baby’s Position
This means the baby’s position in the womb. Is it looking at your belly button, or your spine.
If the baby is positioned looking up — it sometimes takes longer. However, babies can spin at any time.
Honestly, that’s the good news on all of these things. Babies drop or move or change and can advance your labor quickly at any time (or they can stay the same… such is mother nature, right)?
NOTE: If Baby isn’t head down that is called breech positioning and normally requires a cesarean section.
Now, most often (but not always) — as you get closer to your due date, you are more likely to be “favorable‘ in these areas. So, a woman who is at 41 weeks of pregnancy most often has a more favorable cervix (and will have a quicker induction) than someone who is 37 weeks (where labor may take a long time). However, if you’re being induced early (especially for medical reasons) it may not be favorable — and that is OK too, we work with that frequently in the hospital.
As a note, most often first-time mothers take less time also, so all of those things will be considered before an induction of labor by your health care provider.
And finally, remember that ALL these things are just guesses based on statistics — who knows what will happen for you and your birth!
This is a lot to understand, and frankly — it’s even the half of it. I can get your prepared for ALL of it in just a few easy hours in here.
Have you checked a birth class off your to do list✅? I have a few I recommend:
❤️ Best class for couples {per BabyList}
👩💻 Best class available on demand
⚡ Best class JUST for pain management
👶 Best Postpartum-Only Prep
❤️🧡💛💚💙💜 My favorite class is here.
Now is the time to get started!
Problems With an Unfavorable Cervix
When doctors schedule an induction, they consider how “favorable” your cervix is.
That is an over-generalization of the items I mentioned (that are also in your bishop’s score).
If your cervix isn’t favorable (or if your bishop’s score is low) it means that it will likely take longer for your induction.
And, the longer an induction takes, the more medication we have to use, the higher risk you become as you labor longer and longer.
So, obviously we would prefer that you have a favorable cervix coming in.
However, if your induction is medically necessary (see below) it doesn’t matter how favorable it is, as we NEED to have the baby out!
Want to know more about inductions? — check out these posts:
- 5 Things NOT to do Before Your Induction
- Pitocin to Induce Labor
- Inducing Labor at 39 Weeks: Pros and Cons
- 5 Reasons to NOT Get Induced
- What Happens if Your Induction Doesn’t Work?
Prior Obstetrical History
If you’ve previously had a vaginal delivery, it normally takes less time for subsequent babies. Not always though, especially with an early induction — but, usually.
The part that is sped-up the most is the pushing part since your birth canal has already been stretched by a previous head.
How you Respond to the Method of Induction
Just like any medication, some people respond better to them, than others. Some people take a lot, and it’s hard to say if that’s how their body responds to the medicine, or if their body just isn’t ready to have a baby.
BTW, if you’re facing an induction, check out my easy tips to help you prepare for your induction!
Issues With the Baby
If we need to stop/start the induction frequently because of problems with the fetal heart rate that can obviously make your induction take longer. Some babies don’t love contractions or don’t respond well to them, so that is just something we have to take as it comes.
In general, this isn’t super frequent, but it does happen. Also, sometimes mid-induction your baby will show signs of distress, we will stop for a bit and it will resolve.
However, if the stress is too much, they will encourage you to consider a cesarean section. Studies do show that if you are being induced prior to 39 weeks you do increase the risk of a c-section if you are being induced (although if you are being induced prior to 39 weeks there should be a reason for your induction prior to being full-term).
If you’re getting induced early, I have a whole post on what to expect at a 37 week induction!
What did the Arrive Trial Show for Induction Length?
The Arrive trial tested to see if an elective induction at 39 weeks was more risky (for you or baby) than waiting to see if you went into labor on your own. It showed a few things (this is a very surface level review of the study, I go more into in a bonus video in here)
- You were less-likely to have a c-section if you had a 39 week induction rather than waiting to see if you go into labor on your own
- Length of time in labor and delivery was greater if you were induced at 39 weeks, but time in postpartum was less (because less people had a c-section)
- No adverse outcomes were noted for babies being induced earlier.
This study is controversial because it contradicts most of what the labor community has thought prior to it. More studies are coming (although preliminary data backs up this study) — but I think it is an important one to consider. I have a whole bonus video about it in here.
Things Your Providers Can Do to Speed-Up Labor
There are things we can do to speed up your labor. They are done to hopefully create a vaginal delivery.
Make sure you get informed consent before any of these procedures, as each do have potential risks (and benefits).
Membrane Sweep
Your provider will do this in the office after a cervical exam.
It is basically them just using their finger to go between your cervix and your bag of waters.
It is non-invasive and personally I find that it might bump you if you were already close to being in labor. If you weren’t going into labor, it doesn’t do much.
It is mildly painful, but worth a try if you’re 39 weeks and would love to go into labor.
If a membrane sweet is going to work — labor usually starts within 24 hours.
Your doctor may ask you if you want this after about 39 weeks of labor (or, you can ask for it as well).
Foley bulb Insertion
This is where our doctor inserts a tube (called a balloon catheter) up the birth canal into your cervix.
We then fill a balloon at the end of the tube with saline, which slowly stretches open your cervix.
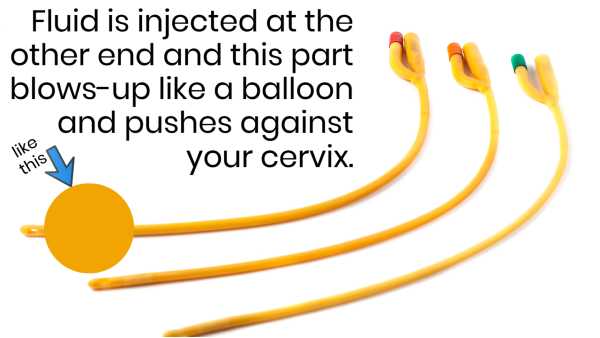
This can be done in your doctor’s office or at the hospital. Fairly non-invasive, and if it doesn’t work it’s not something you can’t walk back from.
It is annoying to have put in, but after that you will likely feel some cramping or contractions with your cervix (hopefully) starting to open.
Your cervix must be somewhat open in order for this to work (otherwise they can’t get the tube into your cervix. In general they use this for 12-24 hours, and then remove it (or sometimes it falls out on its own).
Amniotomy
This is when your healthcare provider breaks your amniotic sac (the nurse can’t do it at the hospital, a obstetrician or a midwife has to do it).
This should be done at the hospital and is an official beginning to labor because once your water breaks we should get the baby out soon (the next day or so) There is always a risk of infection once your water is broken and the baby isn’t protected by that anymore.
Your water can also break at home (although that only happens about 15% of the time).
Breaking your water is often something that doctors do once ou are are already in labor to speed things along.
Induction Agents
These are medications we give that should start uterine contractions (or induce labor). When your provider schedules you as an induction, he/she will likely use one of these methods. They are used very carefully, because at too high of doses they can cause a uterine rupture. They start labor contractions similar to natural labor (vs spontaneous labor).
Cervidil / Cytotec / Prepidil
These are called cervical ripening agents (meaning they ripen your cervix just like you’d ripen an avocado for it to be softer to eat). Some can be given orally, but some are placed using a gloved finger near your cervix. They are prostaglandins (hormones).
These are usually given to soften your cervix, and then you move to…
Pitocin
Is given via IV. It is the same compound your body makes that puts you into labor on its own — the hormone oxytocin (it is just the synthetic version). You can learn more about pitocin.
What if These Induction Agents Don’t Work?
In that event (and it does happen) — we have to ask ourselves:
- Does the baby medically need to come out (in which case you’d need a cesarean delivery)
- Could we wait a bit longer and try again (in which case you might go home).
Your induction may need to be postponed until your body is more ready.
DIY Induction Methods
Many women take castor oil, or try other things to start their labor. Studies & experience show that things like this (particularly castor oil) can be very problematic, and don’t often work — so be mindful before you try an induction of your own.
Things you can do to speed up labor:
There are things you can do to help speed up labor….
Delay Epidural
It seems smart to just come in and get your epidural the minute you get your induction so that you won’t have to feel any pain.
I feel like there is a benefit to your body feeling some pain before you get the epidural.
This allows you to move more and possibly walk or sit on a labor ball to help baby find the best position.
Movement & Position Changes
As I said above, movement and position changes can help the baby find its best spot for delivery.
Some patients are unwilling to change positions. Sometimes some nurses don’t change your position once you have an epidural. I like to move my patients every hour (once they have an epidural).
So, just try to change your position and use movement to your benefit when you have it (even if you’re on pitocin you can often stand by the monitor and move in sexy hip circles or use a stool or a yoga ball).
Changing positions is so important I have cards that help you find your best spots in here.
Elective vs Medically Necessary Inductions
An elective induction is something you are choosing to do. Reasons can be:
- You have childcare for a specific day
- Your husband can come on a specific day
- Your doctor is available on a specific day
- Your doctor just thinks you should have the baby
- You are tired or miserable being pregnant with no specific medical issues.
Medically Necessary Inductions
Often medically necessary inductions happen before you are due. I have a whole post on 37 week inductions.
These are done because providers feel baby’s health will be better outside your womb, than inside.
A medically necessary induction can happen for a variety of reasons — I go into the vast majority of reasons in My Online Course, but the top few are:
Diabetes
Both gestational diabetes and type 1 or 2 diabetes can be a reason to be induced early as baby might be bigger, and you have an increased risk with pregnancy.
Baby Size
The baby’s size can always be a indicator to be induced.
Large Baby
If the baby is getting too large, it might not come out of your pelvis.
Small Baby
If the baby isn’t growing as it should, it is likely that we can help it grow better outside.
Too Much / Too Little Fluid
Oligohydramnios
This means that you have too little amniotic fluid. This can be problematic because baby needs to be surrounded by fluid to both protect it and the cord (and cushion it so it doesn’t get squished).
Polyhydramnios
This means you have too much amniotic fluid. This can be a problem to over-stretch your uterus, or too much room for baby.
Preeclampisa
This is a disorder of your smooth muscle caused by something in the baby/placental development. It is often characterized by high blood pressure or lab work changes with our urine and blood.
That means the only way to stop it is to get the baby out.
Which, is why you might need to be induced.
Other Reasons
Like I said, there are a lot of reasons why a doctor will induce you — these are just the most common.
Alright, so hopefully you understand that all of these come together to show how long your induction will likely be.
Is your hospital bag packed? — I have a handy packing list right here:
Textbook Labor Plan
If your baby read the textbook — it would know that average labor progresses about 1 cm per hour and then pushing begins.
However, most babies don’t read that book and labor can be tricky.
I find that the first 5 centimeters go longer than the last 5.
I also find that none of this starts until you’re actually IN LABOR (called active labor), and sometimes it takes a while to get there (often based on how thick or firm your cervix is).
Active labor is defined as the point when your cervix is dilating at least 1 cm’ish/hour.
With all that being said, if you’re induced early, an induction can sometimes even take 2-3 days, but if you’re induced after 40 weeks and have a very favorable cervix your baby could be out in just a few hours.
Which, I realize isn’t helpful at all. There is no shame in asking your doctor how long they think it will take (believe me, they have an educated guess), or asking your nurse once you’re in labor (it’s hard to tell until you’re in active labor and actually changing your cervix).
Length of Induction FAQ’s
In the study previously referenced first time moms seemed to take about 5 hours longer than those who had previously had a vaginal delivery. However, a lot of it depends on your cervical readiness also.
Honestly, as long as it needs to. As long as you and baby are doing fine during an induction I have seen it take days — often we will stop it, give your body some time to re-group and then re-start it. This would be in a medically necessary case though, where baby needs to come out. If it was an elective induction we would likely send you home and schedule you for a few days from now to see if your body is more ready.
In the arrive trial (I got into that with a whole bonus video about that in here) it showed that induced and non-induced women rated their pain about the same. That is honestly the only study I’ve seen about it. The rest is just thoughts from the birth community. Personally, as someone who has had both I think an induction is more boring (and annoying to be in the hospital) but they hurt similarly.
If you go by the textbook case of labor it is 1 cm/hour plus pushing time. However, that is once you start labor. If you’re not yet in labor you can’t really give a guess until you are in labor (meaning you are having frequent contractions that are opening your cervix).
About 19 hours, if started with Dinoprostone (Cervidil) per this study.
Honestly, if your cervix is ready and your body takes well to the medication it doesn’t always take that long. It really depends on those factors for how long it starts. Remember your body is not ready to go into labor (otherwise it would) so sometimes you’re forcing something it does not want.
AND, finally — I am a big fan of letting mother nature take the lead and going into labor on your own. If you can avoid an induction I would recommend that if at all possible, mostly because of the length of time that an induction on a an un-ready cervix can take. But, sometimes you can’t avoid it, so hopefully this article gave you some good info as well!
I know this all seems very complicated, but it really isn’t. Let me help simplify it for you in The Online Prenatal Class for Couples. In just a few hours I can have you totally prepared for birth.

OR, if you can’t even fit that in, check out Inductions Made Easy where I can get you ready for the induction side of things in under 30-minutes.
Source:
- Zhao L, Lin Y, Jiang T, Wang L, Li M, Wang Y, Sun G, Xiao M. Prediction of the induction to delivery time interval in vaginal dinoprostone-induced labor: a retrospective study in a Chinese tertiary maternity hospital. J Int Med Res. 2019 Jun;47(6):2647-2654. doi: 10.1177/0300060519845780. Epub 2019 May 17. PMID: 31096809; PMCID: PMC6567707.





 Belly Button Pain During Pregnancy (Second Trimester)
Belly Button Pain During Pregnancy (Second Trimester)

[…] it may feel like it hurts more, or that it takes longer. Often you’re starting behind the ball without all those “practice” contractions […]